
Antidepressant-Induced Mania Tied to Mitochondrial Action
[ad_1]
Supply: Nick Youngson/Wikimedia Commons.
When I was identified with bipolar I condition, I was in the midst of a extreme manic episode with psychotic characteristics. I was rail-slim and training fanatically—even in the middle of the evening at a 24-hour fitness center. I slept as minimal as 15 minutes a night, and when I did snooze, I would wake up with my dresses and mattress drenched in sweat. I knowledgeable delusions of grandeur and hyper-religiosity, as very well as heightened senses and creativeness, between other common signs and symptoms of mania.
In retrospect, I had seasoned manic and hypomanic episodes before—I just failed to understand it at the time. For almost 20 decades, my bipolar dysfunction had been misdiagnosed and I experienced been addressed for big depressive disorder and anxiety, for which I experienced experimented with a range of various combos of medicines. When that intense manic episode took keep, I had been using the antidepressants Wellbutrin (bupropion) and Pristiq (desvenlafaxine). For individuals with bipolar ailment, these medication are every single identified to induce mania on their own—and I took them alongside one another. Insert in stressors this sort of as an unappealing divorce, estrangement from my daughters, and recovery from liquor abuse, and it seemed like all roads have been top me to mania.
But why are some antidepressants involved with inducing mania but not some others? A new analyze by a workforce of scientists led by Manuel Gardea-Resendez, M.D., of the Mayo Clinic delivers some intriguing responses.
Resource: Laboratoires Servier/Wikimedia Commons.
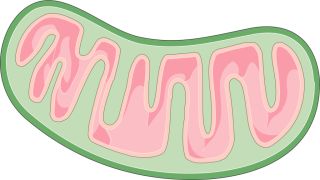
Bipolar Ailment and the Powerhouse of the Cell
About the previous 20 many years, mounting proof has pointed to the involvement of mitochondrial dysfunction in the etiology of bipolar problem. The basic purpose for mitochondria is to create energy by a method referred to as oxidative phosphorylation, which relies in aspect on a set of electron transport chain (Etcetera) proteins. Lessened expression of mitochondrial Etc genes has been persistently uncovered in the frontal cortex and hippocampus of clients with bipolar disorder, and impaired mitochondrial functionality has been implicated in a variety of facets of bipolar problem, such as possibility for shifting into mania and/or psychosis.
Some antidepressants have been demonstrated to maximize Etcetera exercise although others have been demonstrated to reduce And so on exercise. This led scientists to assess no matter if antidepressants that improve mitochondrial activity are involved with greater charges of antidepressant-induced mania (also identified as therapy-emergent mania). Research contributors were picked based on their background of antidepressant exposure and availability of clinical consequence steps.
Immediately after modifying for age, sex, and subtype of bipolar condition, scientists found that therapy-emergent mania was a lot more than two times as frequent in clients uncovered to antidepressants that maximize mitochondrial energetics in contrast to members exposed to antidepressants that decrease mitochondrial exercise.
In addition, their conclusions propose that the categorization of antidepressants based on mitochondrial energetics has medical benefit, as a substitute of common categorization dependent solely on monoaminergic mechanism of motion (e.g., selective serotonin reuptake inhibitors (SSRIs), serotonin norepinephrine reuptake inhibitors (SNRIs), norepinephrine dopamine reuptake inhibitors (NDRIs), and tricyclic antidepressants (TCAs)). Particularly, paroxetine (SSRI), nortriptyline (TCA), bupropion (NDRI), venlafaxine (SNRI), and imipramine (TCA) were found to maximize mitochondrial Etcetera action, when compared to amitriptyline (TCA) and escitalopram (SSRI), which lessened mitochondrial Etcetera action.
Conclusion
Effects from this study give help for the notion that amplified mitochondrial energetics in response to choose antidepressants drives, at least in aspect, the pathophysiology of treatment-emergent mania. As stated by Gardea-Resendez, “Foreseeable future clinical research should look into probable interactions involving mitochondrial mechanisms of illness risk that may predispose to antidepressant related treatment-emergent mania and may have a clear impact on the administration and remedy of patients with bipolar problem.”
[ad_2]
Source hyperlink


